Hemophilia
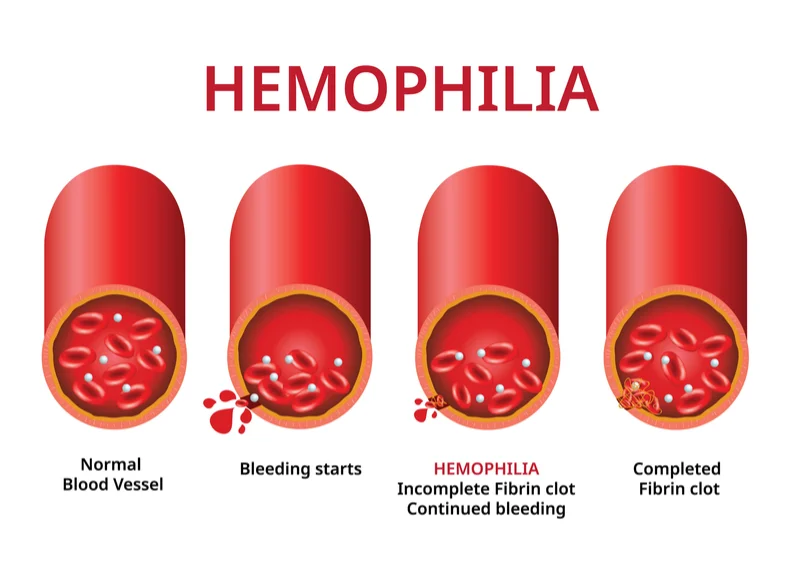
Hemophilia is usually an inherited bleeding disorder in which the blood does not clot properly. This can lead to spontaneous bleeding as well as bleeding following injuries or surgery. Blood contains many proteins called clotting factors that can help to stop bleeding. People with hemophilia have low levels of either factor VIII (8) or factor IX (9). The severity of hemophilia that a person has is determined by the amount of factors in the blood. The lower the amount of the factor, the more likely it is that bleeding will occur which can lead to serious health problems.
Types of hemophilia
Type A
Hemophilia type A is caused by a missing or defective factor VIII protein. It has three stages depending on the ratio of clotting protein in the blood: mild, moderate, and severe. People with hemophilia A bleed longer than others, internally or externally. Those with mild cases generally bleed only after serious injury, trauma, or surgery. Often, the disease is diagnosed after one of these situations due to prolonged bleeding, and the first episode may occur only in adulthood.
Type B
Hemophilia type B is caused by a missing or defective factor IX clotting protein. This type is rarer than type A; however, the severity and symptoms are similar. A subtype of hemophilia type B, known as hemophilia B Leyden, causes episodes of excessive bleeding in childhood, which gradually disappear after puberty.
Type C
Hemophilia type C is caused by a missing or defective factor XI clotting protein. Unlike hemophilia A and B, symptoms don’t correlate with factor XI levels in the blood. People with lower levels may bleed less than those with higher levels of clotting protein. Patients often experience nosebleeds or soft tissue bleeds, as well as hemorrhaging after tooth extraction. Factor XI concentrates are unavailable in the U.S. as yet, so doctors normally treat hemophilia C with fresh frozen plasma.
Acquired Hemophilia
Acquired hemophilia is an autoimmune disorder in which the body’s immune system mistakes self-proteins as foreign and starts producing antibodies against them. In this type of hemophilia, the immune system mistakes the blood clotting protein called factor VIII as foreign and starts to produce antibodies against it. As a result, factor VIII activity is inhibited, which leads to excessive bleeding.
Symptoms of hemophilia
Common signs of hemophilia include:(3)
- bruising
- hematomas, which is when there is bleeding into the muscle or soft tissues
- bleeding from the mouth and gums
- bleeding after a circumcision
- blood in the stool
- blood in the urine
- nosebleeds that are frequent and difficult to stop
- bleeding after vaccinations or other injections
- bleeding into the joints
According to the National Organization for Rare Disorders, the severity of hemophilia can also affect symptoms.
In mild cases, a person will most likely experience:(3)
- spontaneous nose bleeds
- bleeding from the mouth or gums
- easy bruising or hematomas
- excessive bleeding following dental or other surgical procedures or injury
Symptoms for people living with the mild form may not show until adulthood.
In moderate cases of hemophilia, a person may experience:
- easy and excessive bruising
- excessive bleeding following surgeries or trauma
In severe cases of hemophilia, a person may experience spontaneous bleeding, often in the muscles or joints. This can lead to pain and swelling.
Without treatment, it can result in arthritis in the affected joints. Doctors can often diagnose severe cases when the person is an infant
causes of hemophilia
Certain genes create clotting factors. In inherited hemophilia, the genes carrying instructions for making normal clotting factors mutate or change. The mutated genes may give instructions that end up making abnormal clotting factors or not enough clotting factors. That said, about 20% of all hemophilia cases are spontaneous, meaning someone has the disease even though there’s no family history of abnormal bleeding.(1)
Risk factors
The biggest risk factor for hemophilia is having family members who also have the disorder. Males are much more likely to have hemophilia than females.(4)
How do healthcare providers diagnose hemophilia?
A healthcare provider will start by doing a complete history and physical examination. If you have hemophilia symptoms, the provider will ask about your family’s medical history. Providers may do the following tests:(5)
- Complete blood count (CBC): Providers use this test to measure and study blood cells.
- Prothrombin time (PT) test: Providers use this test to see how quickly your blood clots.
- Activated partial thromboplastin time test: This is another blood test to time blood clot formation.
- Specific clotting factor test(s): This blood test show levels of specific clotting factor levels (such as factor 8 and factor 9).
Treatment
The main treatment for severe hemophilia involves replacing the clotting factor you need through a tube in a vein.
This replacement therapy can be given to treat a bleeding episode in progress. It can also be given on a regular schedule at home to help prevent bleeding episodes. Some people receive continuous replacement therapy.(6)
Replacement clotting factor can be made from donated blood. Similar products called recombinant clotting factors, are made in a laboratory, not from human blood.
Other therapies include:(6,7)
- Desmopressin. In some forms of mild hemophilia, this hormone can stimulate the body to release more clotting factors. It can be injected slowly into a vein or used as a nasal spray.
- Emicizumab (Hemlibra). This is a newer drug that doesn't include clotting factors. This drug can help prevent bleeding episodes in people with hemophilia A.
- Clot-preserving medications. Also known as anti-fibrinolytic, these medications help prevent clots from breaking down.
- Fibrin sealants. These can be applied directly to wound sites to promote clotting and healing. Fibrin sealants are especially useful for dental work.
- Physical therapy. It can ease signs and symptoms if internal bleeding has damaged your joints. Severe damage might require surgery.
First aid for minor cuts. Using pressure and a bandage will generally take care of the bleeding. For small areas of bleeding beneath the skin, use an ice pack. Ice pops can be used to slow down minor bleeding in the mouth.
Living with hemophilia
With treatment, most people with hemophilia can live a normal life.
However, you should:(8)
- avoid contact sports, such as rugby
- be careful taking other medicines – some can affect your blood's ability to clot, such as aspirin and ibuprofen
- take care of your teeth and gums and have regular check-ups at the dentist
Looking after your teeth and gums helps you avoid problems such as gum disease, which can cause bleeding. Most non-surgical dental treatment can be done at a general dental surgery.
Food to eat and avoid with hemophilia:(9)
1: Iron-rich food
Maintaining iron levels is particularly important for people with hemophilia, as an estimated 0,75 micrograms of iron is lost with each 15 ml of blood. Iron-rich foods include liver, lean red meat, poultry, and leafy green vegetables such as spinach, broccoli, dried beans, grains, and raisins. Combining iron-rich foods with good sources of vitamin C can enhance iron absorption by the body.
2: Whole grains
Increasing your whole grain intake – making half of your grain consumption come from oats, barley, whole wheat, bran, brown rice, or pasta is a good way to satiate your appetite, lower your cholesterol, and stabilize blood glucose levels.
3: Low-fat or no fat
Switching to low-fat dairy products – skimmed milk or low-fat cheeses- are good sources of vitamins and minerals as well as calcium, without the unnecessary fats. Also: reduce your fat intake by choosing baking, boiling, or grilling instead of frying. And use vegetable oils over butter or animal fats.
4: Avoid hidden sugars and fatteners
Many people don’t realize how much sugar is contained in soft drinks, but also ‘healthy’ fruit juices can be full of calories and sugar. Especially notorious are smoothies and yogurt shakes. Also risky are salad dressings and condiments: have them on the side if possible. And choose mustard instead of mayonnaise or ketchup: mustard mostly consists of vinegar.
5: Be careful with supplements
If you are considering dietary supplements, discuss your choices with your doctor before taking any supplements, as some might increase bleeding tendency or clotting times in the same way as aspirin or non-steroidal anti-inflammatories do. Some supplements — such as vitamin E, fish oil, ginkgo biloba, bromelain, flax seed, garlic, or ginger — may need to be avoided altogether.
causes of hemophilia
Certain genes create clotting factors. In inherited hemophilia, the genes carrying instructions for making normal clotting factors mutate or change. The mutated genes may give instructions that end up making abnormal clotting factors or not enough clotting factors. That said, about 20% of all hemophilia cases are spontaneous, meaning someone has the disease even though there’s no family history of abnormal bleeding.(1)
Risk factors
The biggest risk factor for hemophilia is having family members who also have the disorder. Males are much more likely to have hemophilia than females.(4)
How do healthcare providers diagnose hemophilia?
A healthcare provider will start by doing a complete history and physical examination. If you have hemophilia symptoms, the provider will ask about your family’s medical history. Providers may do the following tests:(5)
- Complete blood count (CBC): Providers use this test to measure and study blood cells.
- Prothrombin time (PT) test: Providers use this test to see how quickly your blood clots.
- Activated partial thromboplastin time test: This is another blood test to time blood clot formation.
- Specific clotting factor test(s): This blood test show levels of specific clotting factor levels (such as factor 8 and factor 9).
Treatment
The main treatment for severe hemophilia involves replacing the clotting factor you need through a tube in a vein.
This replacement therapy can be given to treat a bleeding episode in progress. It can also be given on a regular schedule at home to help prevent bleeding episodes. Some people receive continuous replacement therapy.(6)
Replacement clotting factor can be made from donated blood. Similar products called recombinant clotting factors, are made in a laboratory, not from human blood.
Other therapies include:(6,7)
- Desmopressin. In some forms of mild hemophilia, this hormone can stimulate the body to release more clotting factors. It can be injected slowly into a vein or used as a nasal spray.
- Emicizumab (Hemlibra). This is a newer drug that doesn't include clotting factors. This drug can help prevent bleeding episodes in people with hemophilia A.
- Clot-preserving medications. Also known as anti-fibrinolytic, these medications help prevent clots from breaking down.
- Fibrin sealants. These can be applied directly to wound sites to promote clotting and healing. Fibrin sealants are especially useful for dental work.
- Physical therapy. It can ease signs and symptoms if internal bleeding has damaged your joints. Severe damage might require surgery.
First aid for minor cuts. Using pressure and a bandage will generally take care of the bleeding. For small areas of bleeding beneath the skin, use an ice pack. Ice pops can be used to slow down minor bleeding in the mouth.
Living with hemophilia
With treatment, most people with hemophilia can live a normal life.
However, you should:(8)
- avoid contact sports, such as rugby
- be careful taking other medicines – some can affect your blood's ability to clot, such as aspirin and ibuprofen
- take care of your teeth and gums and have regular check-ups at the dentist
Looking after your teeth and gums helps you avoid problems such as gum disease, which can cause bleeding. Most non-surgical dental treatment can be done at a general dental surgery.
Food to eat and avoid with hemophilia:(9)
1: Iron-rich food
Maintaining iron levels is particularly important for people with hemophilia, as an estimated 0,75 micrograms of iron is lost with each 15 ml of blood. Iron-rich foods include liver, lean red meat, poultry, and leafy green vegetables such as spinach, broccoli, dried beans, grains, and raisins. Combining iron-rich foods with good sources of vitamin C can enhance iron absorption by the body.
2: Whole grains
Increasing your whole grain intake – making half of your grain consumption come from oats, barley, whole wheat, bran, brown rice, or pasta is a good way to satiate your appetite, lower your cholesterol, and stabilize blood glucose levels.
3: Low-fat or no fat
Switching to low-fat dairy products – skimmed milk or low-fat cheeses- are good sources of vitamins and minerals as well as calcium, without the unnecessary fats. Also: reduce your fat intake by choosing baking, boiling, or grilling instead of frying. And use vegetable oils over butter or animal fats.
4: Avoid hidden sugars and fatteners
Many people don’t realize how much sugar is contained in soft drinks, but also ‘healthy’ fruit juices can be full of calories and sugar. Especially notorious are smoothies and yogurt shakes. Also risky are salad dressings and condiments: have them on the side if possible. And choose mustard instead of mayonnaise or ketchup: mustard mostly consists of vinegar.
5: Be careful with supplements
If you are considering dietary supplements, discuss your choices with your doctor before taking any supplements, as some might increase bleeding tendency or clotting times in the same way as aspirin or non-steroidal anti-inflammatories do. Some supplements — such as vitamin E, fish oil, ginkgo biloba, bromelain, flax seed, garlic, or ginger — may need to be avoided altogether.
References:
1. What is Hemophilia | CDC [Internet]. [cited 2023 Jul 6]. Available from: https://www.cdc.gov/ncbddd/hemophilia/facts.html
2. Types of Hemophilia - Hemophilia News Today [Internet]. [cited 2023 Jul 6]. Available from: https://hemophilianewstoday.com/types-of-hemophilia-2/
3. Hemophilia: Causes, types, symptoms, and treatment [Internet]. [cited 2023 Jul 6]. Available from: https://www.medicalnewstoday.com/articles/154880#symptoms
4. Hemophilia - Symptoms and causes - Mayo Clinic [Internet]. [cited 2023 Jul 6]. Available from: https://www.mayoclinic.org/diseases-conditions/hemophilia/symptoms-causes/syc-20373327
5. Diagnosis of Hemophilia | CDC [Internet]. [cited 2023 Jul 6]. Available from: https://www.cdc.gov/ncbddd/hemophilia/diagnosis.html
6. Hemophilia - Diagnosis and treatment - Mayo Clinic [Internet]. [cited 2023 Jul 6]. Available from: https://www.mayoclinic.org/diseases-conditions/hemophilia/diagnosis-treatment/drc-20373333
7. Weyand AC, Pipe SW. New therapies for hemophilia. Blood. 2019 Jan 31;133(5):389–98.
8. Haemophilia - NHS [Internet]. [cited 2023 Jul 6]. Available from: https://www.nhs.uk/conditions/haemophilia/
9. Haemophilia: five things to eat and five things to avoid - BJH [Internet]. [cited 2023 Jul 6]. Available from: https://www.bjh.be/haemophilia-five-things-to-eat-and-five-things-to-avoid/