When you’re on your way to a shopping mall, do you think about the exact location of each toilet before you get there? And when you are out and laughing with your friends, do you hold back your laughter for fear of getting your clothes wet (with urine)? And when you put the key in the lock of the door of your house or apartment, do you feel confused by the uncontrollable urge to urinate? Does urine leak when you cough or sneeze?
If you answered yes to any of these questions, you may have urinary incontinence.
Urinary incontinence is the leaking of urine that you can’t control. Many people suffer from urinary incontinence. We don’t know for sure exactly how many. That’s because many people do not tell anyone about their symptoms. They may be embarrassed, or they may think nothing can be done. So they suffer in silence.(1)
Urinary incontinence is not just a medical problem. It can affect emotional, psychological, and social life. Many people who have urinary incontinence are afraid to do normal daily activities. They don’t want to be too far from a toilet. Urinary incontinence can keep people from enjoying life.
Many people think urinary incontinence is just part of getting older. But it’s not. And it can be managed or treated.
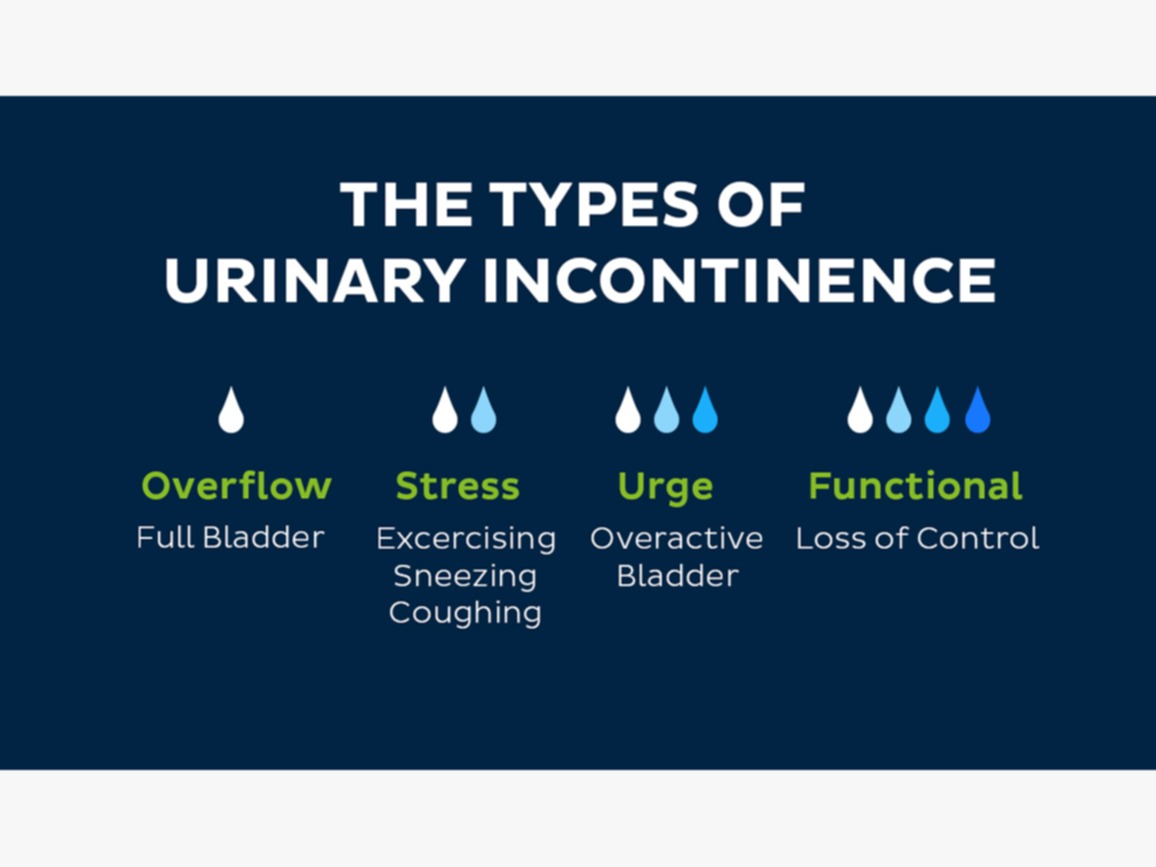
Types of urinary incontinence include:(2)
- Stress incontinence: Urine leaks when you exert pressure on your bladder by coughing, sneezing, laughing, exercising, or lifting something heavy.
- Urge incontinence: You have a sudden, intense urge to urinate followed by an involuntary loss of urine. You may need to urinate often, including throughout the night. Urge incontinence may be caused by a minor condition, such as infection, or a more severe condition such as a neurological disorder or diabetes.
- Overflow incontinence: You experience frequent or constant dribbling of urine due to a bladder that doesn’t empty.
- Functional incontinence: A physical or mental impairment keeps you from making it to the toilet in time. For example, if you have severe arthritis, you may not be able to unbutton your pants quickly enough.
- Mixed incontinence: You experience more than one type of urinary incontinence — most often this refers to a combination of stress incontinence and urges incontinence.
You may feel uncomfortable discussing incontinence with your doctor. But if incontinence is frequent or is affecting your quality of life, it’s important to seek medical advice because urinary incontinence may:(2)
- Cause you to restrict your activities and limit your social interactions
- Negatively impact your quality of life
- Increase the risk of falls in older adults as they rush to the toilet
- Indicate a more serious underlying condition
Causes of urinary incontinence
Chronic or long-term causes of incontinence can include:(3)
- Pelvic floor disorders: When you have an issue with your pelvic floor muscles, it can impact the way your organs function, including your bladder.
- Stroke: A stroke can cause you to experience issues with muscle control. This can include the muscles that regulate your urinary system.
- Diabetes: When you have diabetes, your body produces more urine. This increase in the amount of urine can cause leakage issues. In addition, peripheral neuropathy can affect the bladder’s function.
- Menopause: Menopause is another time of change in a woman’s body when hormone levels change rapidly and pelvic floor muscles can also become weaker — something that also can happen as you get older.
- Multiple sclerosis (MS): If you have MS, you may experience a loss of control of your bladder, leading to leakage issues.
- Enlarged prostate: When the prostate is larger than normal, it can cause several bladder control issues. You might also hear this condition called benign prostatic hyperplasia, or BPH.
- After prostate cancer surgery: During prostate cancer surgery the sphincter muscle can sometimes be damaged leading to stress incontinence.
Why does pregnancy cause incontinence?(3)
During pregnancy, your body goes through a lot of physical changes. As your uterus stretches to hold the growing baby, a few things happen. Your bladder can be squished by the expanding baby, making your bladder hold less than before. You might experience an increased urgency to pee during pregnancy because your bladder cannot hold as much as before. This might become even more challenging towards the end of pregnancy when the baby is at its largest.
Another reason for incontinence during pregnancy is the weakening of your pelvic floor muscles. These muscles are the support structures for all of the organs in your pelvis. During pregnancy, they can be stretched and weakened as your uterus expands.
Signs and Symptoms of Urinary Incontinence(4)
- Leaking urine during normal activities like lifting, bending, coughing, or exercising(5)
- Sudden, strong urges to urinate, or feeling like you might not make it to the toilet in time
- Leaking urine without feeling any warning signs or urge
- Bed-wetting
Treatment
Treatment will depend on several factors, such as the type of incontinence, the patient’s age, general health, and mental state.
Stress incontinence
Pelvic floor exercises, also known as Kegel exercises, help strengthen the urinary sphincter and pelvic floor muscles – the muscles that help control urination.(5)
Bladder training(5)
- Delaying the event: The aim is to control the urge. The patient learns how to delay urination whenever there is an urge to do so.
- Double voiding: This involves urinating, then waiting for a couple of minutes, then urinating again.
- Toilet timetable: The person schedules the bathroom at set times during the day, for example, every 2 hours.
Bladder training helps the patient gradually regain control over their bladder.
Medications for urinary incontinence
If medications are used, this is usually in combination with other techniques or exercises.
The following medications are prescribed to treat urinary incontinence:(5)
- Anticholinergics calm overactive bladders and may help patients with urge incontinence.
- Topical estrogen may reinforce tissue in the urethra and vaginal areas and lessen some of the symptoms.
Imipramine (Tofranil) is a tricyclic antidepressant.
Medical devices
The following medical devices are designed for females.(5)
- Urethral inserts: A woman inserts the device before activity and takes it out when she wants to urinate.
- Pessary: A rigid ring inserted into the vagina and worn all day. It helps hold the bladder up and prevent leakage.
- Radiofrequency therapy: Tissue in the lower urinary tract is heated. When it heals, it is usually firmer, often resulting in better urinary control.
- Botox (botulinum toxin type A): Injected into the bladder muscle, this can help those with an overactive bladder.
- Bulking agents: Injected into the tissue around the urethra, these help keep the urethra closed.
- Sacral nerve stimulator: This is implanted under the skin of the buttock. A wire connects it to a nerve that runs from the spinal cord to the bladder. The wire emits an electrical pulse that stimulates the nerve, helping bladder control.
Surgery(5)
Surgery is an option if other therapies do not work. Women who plan to have children should discuss surgical options with a doctor before making the decision.
- Sling procedures: A mesh is inserted under the neck of the bladder to help support the urethra and stop urine from leaking out.
- Colpo suspension: Lifting the bladder neck can help relieve stress incontinence.
- Artificial sphincter: An artificial sphincter, or valve, may be inserted to control the flow of urine from the bladder into the urethra.
Supplements for Incontinence
Magnesium
Magnesium helps your body with a host of functions, including lowering high blood pressure, regulating mood, and helping to guard against Type 2 diabetes. It also ensures our muscles and nerves function properly, and some experts believe that it may help improve incontinence symptoms by reducing bladder muscle spasms, and allowing the bladder to empty.(6)
sources of magnesium: bananas, avocados, black beans, cooked quinoa, certain fish, dark leafy greens, nuts, and seeds.
Using Supplements for Diabetes Treatment
According to the American Diabetes Association, diabetics are more likely to use supplements than those without the disease.(9)
Supplements should not be used to replace standard diabetes treatment. Doing so can put your health at risk.
It is important to talk to your doctor before using any supplements. Some of these products can interfere with other treatments and medications. Just because a product is natural does not mean it is safe to use.
Cinnamon
A study has shown that cinnamon, in whole form or extract, helps lower fasting blood glucose levels(9)
Chromium
Chromium is an essential trace element. It is used in the metabolism of carbohydrates. However, research on the use of chromium for diabetes treatment is mixed. Low doses are safe for most people, but there is a risk that chromium could make blood sugar go too low. High doses also have the potential to cause kidney damage.(9)
Green Tea
Green tea contains polyphenols, which are antioxidants.
The main antioxidant in green tea is known as epigallocatechin gallate (EGCG). Laboratory studies have suggested that EGCG may have numerous health benefits including:(9)
- lower cardiovascular disease risk
- prevention of type 2 diabetes
- improved glucose control
- better insulin activity
Magnesium
Magnesium is an essential nutrient. It helps regulate blood pressure. It also regulates insulin sensitivity. Supplemental magnesium may improve insulin sensitivity in diabetics.
A high magnesium diet may also reduce the risk of diabetes. Researchers have found a link between higher magnesium intake, lower rates of insulin resistance, and diabetes.(9)
Makkah Pharmacy recommends:
Vitamin D
Vitamin D is known to help with bone health, as well as the immune system, heart health, blood sugar levels, and mood regulation. Studies have also found that vitamin D deficiency is associated with a higher risk of pelvic floor disorders. And, in one study of older women, the risk of developing urinary incontinence was 45% lower among those with normal vitamin D levels. (6)
The best way to get most of the vitamin D you need is from sun exposure, but it’s also found in many dairy products, such as milk, yogurt, eggs, fish, and supplements.
Vitamin C
Good sources of Vitamin C can be found in citrus fruits, green and red peppers, broccoli, Brussels sprouts, cauliflower, leafy greens, sweet and white potatoes, and tomatoes (including tomato juice!).(7)
Makkah Pharmacy recommends:
References
1. Incontinence: Symptoms & Treatment – Urology Care Foundation [Internet]. [cited 2022 Dec 30]. Available from: https://www.urologyhealth.org/urology-a-z/u/urinary-incontinence
2. Urinary incontinence – Symptoms and causes – Mayo Clinic [Internet]. [cited 2022 Dec 30]. Available from: https://www.mayoclinic.org/diseases-conditions/urinary-incontinence/symptoms-causes/syc-20352808
3. Incontinence: Leakage, Causes, Diagnosis, Treatment & Prevention [Internet]. [cited 2022 Dec 30]. Available from: https://my.clevelandclinic.org/health/diseases/17596-urinary-incontinence#symptoms-and-causes
4. What Is Urinary Incontinence? Symptoms, Causes, Diagnosis, Treatment, and Prevention | Everyday Health [Internet]. [cited 2022 Dec 30]. Available from: https://www.everydayhealth.com/urinary-incontinence/guide/
5. Urinary incontinence: Treatment, causes, types, and symptoms [Internet]. [cited 2022 Dec 30]. Available from: https://www.medicalnewstoday.com/articles/165408#treatment
6. Supplements for Incontinence | Incontinence Institute [Internet]. [cited 2022 Dec 30]. Available from: https://myconfidentlife.com/blog/supplements-for-incontinence
7. 3 Vitamins That May Help With Bladder Control – National Association For Continence [Internet]. [cited 2022 Dec 30]. Available from: https://nafc.org/bhealth-blog/3-vitamins-that-may-help-with-bladder-control/







Write a comment
Your email address will not be published. All fields are required