Eye Care
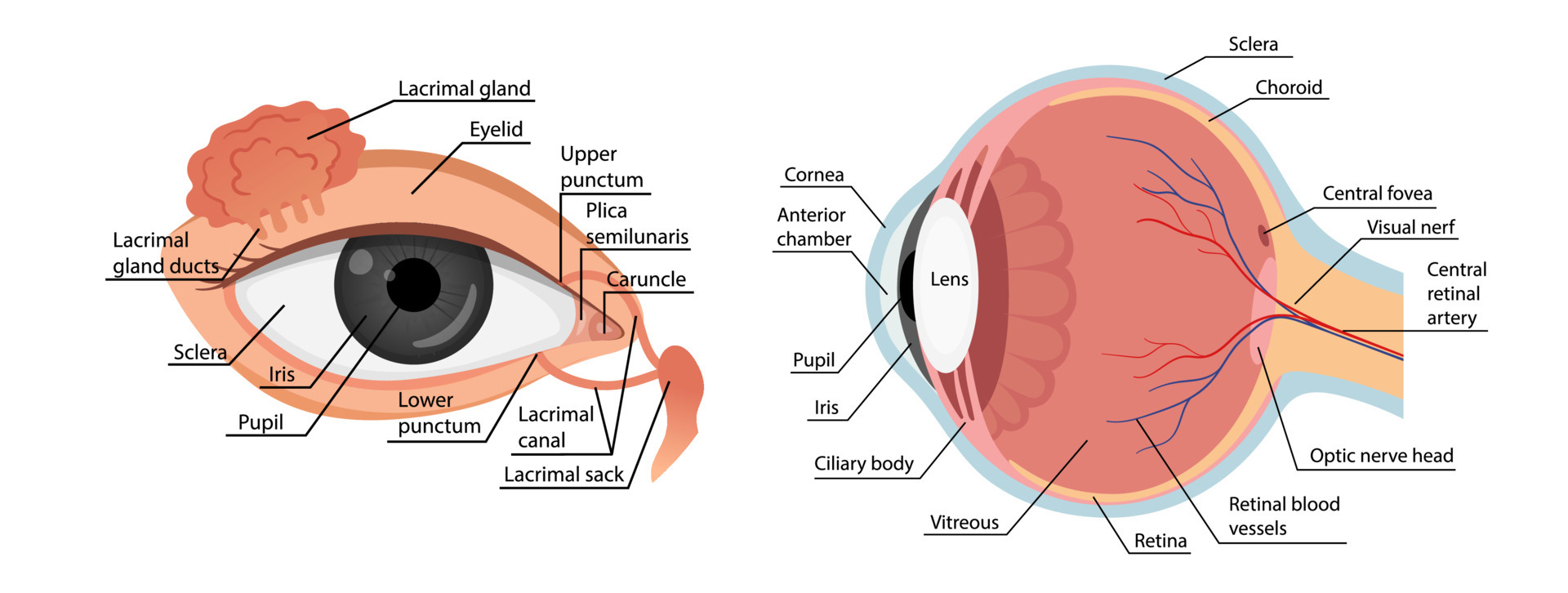
Your eye is a slightly asymmetrical globe, about an inch in diameter. The front part (what you see in the mirror) includes:(1)
- Iris: the colored part
- Cornea: a clear dome over the iris
- Pupil: the black circular opening in the iris that lets light in
- Sclera: the white of your eye
- Conjunctiva: a thin layer of tissue that covers the entire front of your eye, except for the cornea
- Macula: a small area that’s part of the retina. It’s responsible for central vision and helping you see fine details and color.
- Optic Nerve: behind the retina. It carries signals from the retina to your brain, which interprets that visual information to tell you what you are seeing.
- Muscles: control your eye’s position and movement, how much light gets into your eye, and your eyes’ ability to focus.
- Vitreous: a transparent gel that fills your entire eye. It protects and maintains the shape of the eye.
Eye color is created by the amount and type of pigment in your iris. Multiple genes inherited from each parent determine a person’s eye color.(1)
How do your eyes work?
The different parts of your eye work together to help you see images and send visual information to your brain. This process all happens extremely quickly. When you look at an object:(2)
-
- Light enters your eye through the cornea and goes to your lens. Your pupil gets bigger and smaller to control the amount of light that gets into your eye.
- Your cornea and lens refract (bend) the light to bring what you’re seeing into focus.
- Light reaches the retina at the back of your eye, and the retina changes the images into electrical impulses or signals.
- The optic nerve transfers these signals to the part of your brain that’s responsible for vision (visual cortex). The optic nerve carries signals from both eyes at once.
- Your brain interprets what you’ve seen. It combines the visual information from both eyes and brings it all together into one clear image.
What are some common signs or symptoms of eye conditions?
Signs of eye problems include:(2)
- Eye pain, redness, swelling, bleeding, or discharge.
- Eyes that cross or point in different directions.
- Eyes that sting, itch, burn, or are very dry.
- Flashes of light, especially in your peripheral (side) vision.
- Headaches and squinting.
- Inability to move your eyes or open or close your eyelid.
- Many spots or one dark spot in the middle of your field of vision.
- Sensitivity to light or trouble seeing in low light.
- Vision changes, including cloudy or blurry vision and double vision.
Eye conditions
Age-related macular degeneration
Age-related macular degeneration (AMD) is an eye disease that may get worse over time. It’s the leading cause of severe, permanent vision loss in people over 60 years old. (3)
It happens when the small central portion of your retina, called the macula, wears down. The retina is the light-sensing nerve tissue at the back of your eye. (3)
Because the disease happens as you get older, it’s often called age-related macular degeneration. It usually doesn’t cause blindness but might cause severe vision problems.
Symptoms
The first sign you may notice is a gradual or sudden change in the quality of your vision or that straight lines appear distorted to you. This may gradually turn into a dramatic loss of your central vision.(4)
Other symptoms include:(4)
- Dark, blurry areas or whiteouts appear in the center of your vision.
- In rare cases, you may have a change in your perception of color.
Treatment
There's no cure, but treatment for age-related macular degeneration (AMD) may slow the disease and keep you from having serious loss of vision. Dry macular degeneration is the most common type. It’s when the macula – the part of the retina that helps you see straight in front of you – gets thinner as you age. It can advance into wet macular degeneration, which is when blood vessels grow under your retina and leak. (5)
Dry eye
Dry eye disease is a common condition that occurs when your tears can’t provide adequate lubrication for your eyes. Tears can be inadequate and unstable for many reasons. For example, dry eyes may occur if you don't produce enough tears or if you produce poor-quality tears. This tear instability leads to inflammation and damage to the eye's surface. (6)
Dry eyes feel uncomfortable. If you have dry eyes, your eyes may sting or burn. You may experience dry eyes in certain situations, such as on an airplane, in an air-conditioned room, while riding a bike, or after looking at a computer screen for a few hours.
Symptoms
Signs and symptoms, which usually affect both eyes, may include:(7)
- A stinging, burning, or scratchy sensation in your eyes
- Stringy mucus in or around your eyes
- Sensitivity to light
- Eye redness
- A sensation of having something in your eyes
- Difficulty wearing contact lenses
- Difficulty with nighttime driving
- Watery eyes, which is the body's response to the irritation of dry eyes
- Blurred vision or eye fatigue
Treatment
For most people with occasional or mild dry eye symptoms, it's enough to regularly use nonprescription eye drops, also called artificial tears. If your symptoms are persistent and more serious, you have other options. What you do depends on what's causing your dry eyes. (8)
Prescription medicines used to treat dry eyes include:(9)
- Medicines to reduce eyelid inflammation. Inflammation along the edge of your eyelids can keep oil glands from secreting oil into your tears. Your eye care specialist may recommend antibiotics to reduce inflammation. Antibiotics for dry eyes are usually taken by mouth, though some are used as eye drops or ointments.
- Eye drops to control cornea inflammation. Inflammation on the surface of your eyes (cornea) may be controlled with prescription eye drops that contain the immune-suppressing medicine cyclosporine (Restasis) or corticosteroids. Corticosteroids are not ideal for long-term use due to possible side effects.
- Eye inserts that work like artificial tears. If you have moderate to severe dry eye symptoms and artificial tears don't help, another option may be a tiny eye insert that looks like a clear grain of rice. Once a day, you place the hydroxypropyl cellulose (Lacrisert) insert between your lower eyelid and your eyeball. The insert dissolves slowly, releasing a substance that's used in eye drops to lubricate your eye.
- Tear-stimulating medicines. Medicines called cholinergically (pilocarpine, cevimeline) help increases tear production. These medicines are available as pills, gels, or eye drops. Possible side effects include sweating.
- Eye drops made from your blood. These are called autologous blood serum drops. They may be an option if you have severe dry eye symptoms that don't respond to any other treatment. To make these eye drops, a sample of your blood is processed to remove the red blood cells and then mixed with a salt solution.
- A nasal spray to increase tear production. The Food and Drug Administration (FDA) recently approved varenicline (Tyrvaya) to treat dry eyes. This medicine is delivered via a nasal spray. Varenicline is to be sprayed once into each nostril, twice a day.
Glaucoma
Glaucoma is a condition that damages your eye's optic nerve. It gets worse over time. It's often linked to a buildup of pressure inside your eye. Glaucoma tends to run in families. You usually don’t get it until later in life. (10)
The increased pressure in your eye, called intraocular pressure, can damage your optic nerve, which sends images to your brain. If the damage worsens, glaucoma can cause permanent vision loss or even total blindness within a few years.
Risk factor:
You’re more likely to get it if you:(10)
- Are of African American, Irish, Russian, Japanese, Hispanic, Inuit, or Scandinavian descent
- Are over 40
- Have a family history of glaucoma
- Are nearsighted or farsighted
- Have poor vision
- Have diabetes
- Take certain steroid medications such as prednisone
- Take certain drugs for bladder control or seizures, or some over-the-counter cold remedies
- Have had an injury to your eye or eyes
- Have corneas that are thinner than usual
- Have high blood pressure, heart disease, diabetes, or sickle cell anemia
- Have high eye pressure
Symptoms
The symptoms of glaucoma depend on the type and stage of your condition.(11)
Open-angle glaucoma
- No symptoms in the early stages
- Gradually, patchy blind spots in your side vision. Side vision also is known as peripheral vision
- In later stages, difficulty seeing things in your central vision
Acute angle-closure glaucoma
- Severe headache
- Severe eye pain
- Nausea or vomiting
- Blurred vision
- Halos or colored rings around lights
- Eye redness
Normal-tension glaucoma
- No symptoms in the early stages
- Gradually, blurred vision
- In later stages, loss of side vision
Glaucoma in children
- A dull or cloudy eye (infants)
- Increased blinking (infants)
- Tears without crying (infants)
- Blurred vision
- Nearsightedness that gets worse
- Headache
Pigmentary glaucoma
- Halos around lights
- Blurred vision with exercise
- Gradual loss of side vision
Treatment
Glaucoma treatment often starts with prescription eye drops. Some may decrease eye pressure by improving how fluid drains from your eye. Others decrease the amount of fluid your eye makes. Depending on how low your eye pressure needs to be, you may be prescribed more than one eye drop.
Prescription eye drop medicines include:(12)
- Prostaglandins. These increase the outflow of the fluid in your eye, helping to reduce eye pressure. Medicines in this category include latanoprost (Xalatan), travoprost (Travatan Z), tafluprost (Zioptan), bimatoprost (Lumigan) and latanoprostene bunod (Vyzulta).
Possible side effects include mild reddening and stinging of the eyes, darkening of the iris, darkening of the pigment of the eyelashes or eyelid skin, and blurred vision. This class of drug is prescribed for once-a-day use.
- Beta-blockers. These reduce the production of fluid in your eye, helping to lower eye pressure. Examples include timolol (Betimol, Istalol, Timoptic) and betaxolol (Betoptic S).
Possible side effects include difficulty breathing, slowed heart rate, lower blood pressure, impotence, and fatigue. This class of drug can be prescribed for once- or twice-daily use depending on your condition.
- Alpha-adrenergic agonists. These reduce the production of the fluid that flows throughout the inside of your eye. They also increase the outflow of fluid in your eye. Examples include apraclonidine (Iopidine) and brimonidine (Alphagan P, Qoliana).
Possible side effects include irregular heart rate, high blood pressure, fatigue, red, itchy, or swollen eyes, and dry mouth. This class of drug is usually prescribed for twice-daily use but sometimes can be prescribed for use three times a day.
- Carbonic anhydrase inhibitors. These medicines reduce the production of fluid in your eye. Examples include dorzolamide and brinzolamide (Azopt). Possible side effects include a metallic taste, frequent urination, and tingling in the fingers and toes. This class of drug is usually prescribed for twice-daily use but sometimes can be prescribed for use three times a day.
- Rho kinase inhibitor. This medicine lowers eye pressure by suppressing the rho kinase enzymes responsible for the fluid increase. It is available as netarsudil (Rhopressa) and is prescribed for once-a-day use. Possible side effects include eye redness and eye discomfort.
- Miotic or cholinergic agents. These increase the outflow of fluid from your eye. An example is pilocarpine (Isopto Carpine). Side effects include headache, eye ache, smaller pupils, possible blurred or dim vision, and nearsightedness. This class of medicine is usually prescribed to be used up to four times a day. Because of potential side effects and the need for frequent daily use, these medicines are not prescribed very often anymore.
Other treatment options include laser therapy and surgery. The following techniques may help to drain fluid within the eye and lower eye pressure:(12)
- Laser therapy. Laser trabeculoplasty is an option if you can't tolerate eye drops. It also may be used if the medicine hasn't slowed the progression of your disease. Your eye doctor also may recommend laser surgery before using eye drops. It's done in your eye doctor's office. Your eye doctor uses a small laser to improve the drainage of the tissue located at the angle where the iris and cornea meet. It may take a few weeks before the full effect of this procedure becomes apparent.
- Filtering surgery. This is a surgical procedure called a trabeculectomy. The eye surgeon creates an opening in the white of the eye, which also is known as the sclera. The surgery creates another space for fluid to leave the eye.
- Drainage tubes. In this procedure, the eye surgeon inserts a small tube in your eye to drain excess fluid to lower eye pressure.
- Minimally invasive glaucoma surgery (MIGS). Your eye doctor may suggest a MIGS procedure to lower your eye pressure. These procedures generally require less immediate postoperative care and have less risk than trabeculectomy or using a drainage device. They are often combined with cataract surgery. There are a few MIGS techniques available, and your eye doctor will discuss which procedure may be right for you.
Diabetic Retinopathy
Diabetic retinopathy is an eye condition that causes changes to the blood vessels in the part of your eye called the retina. That's the lining at the back of your eye that changes light into images. The blood vessels can swell, leak fluid, or bleed, which often leads to vision changes or blindness. It usually affects both eyes. When left untreated, diabetic retinopathy can scar and damage your retina. (13)
Diabetic retinopathy is the most common cause of vision loss for people with diabetes.
Symptoms
You might not have any signs of diabetic retinopathy until it becomes serious. When you do have symptoms, you might notice:(13)
- Loss of central vision, which is used when you read or drive
- Not being able to see colors
- Blurry vision
- Holes or black spots in your vision
- Floaters, or small spots in your vision caused by bleeding
Risk factors
Anyone who has diabetes can develop diabetic retinopathy. The risk of developing the eye condition can increase as a result of:(14)
- Having diabetes for a long time
- Poor control of your blood sugar level
- High blood pressure
- High cholesterol
- Pregnancy
- Tobacco use
- Being Black, Hispanic, or Native American
Treatment(15)
Early diabetic retinopathy
You might not need treatment immediately if you have mild or moderate nonproliferative diabetic retinopathy. However, your eye doctor will closely monitor your eyes to determine when you might need treatment.
Work with your diabetes doctor (endocrinologist) to determine if there are ways to improve your diabetes management. When diabetic retinopathy is mild or moderate, good blood sugar control can usually slow the progression.
Advanced diabetic retinopathy
If you have proliferative diabetic retinopathy or macular edema, you'll need prompt treatment. Depending on the specific problems with your retina, options might include:
- Injecting medications into the eye. These medications, called vascular endothelial growth factor inhibitors, are injected into the vitreous of the eye. They help stop the growth of new blood vessels and decrease fluid buildup.
Two drugs are approved by the U.S. Food & Drug Administration (FDA) for the treatment of diabetic macular edema — ranibizumab (Lucentis) and aflibercept (Eylea). A third drug, bevacizumab (Avastin), can be used off-label for the treatment of diabetic macular edema.
These drugs are injected using topical anesthesia. The injections can cause mild discomfort, such as burning, tearing, or pain, for 24 hours after the injection. Possible side effects include a buildup of pressure in the eye and infection.
These injections will need to be repeated. In some cases, the medication is used with photocoagulation.
- Photocoagulation. This laser treatment, also known as focal laser treatment, can stop or slow the leakage of blood and fluid in the eye. During the procedure, leaks from abnormal blood vessels are treated with laser burns.
Focal laser treatment is usually done in your doctor's office or eye clinic in a single session. If you had blurred vision from macular edema before surgery, the treatment might not return your vision to normal, but it's likely to reduce the chance of the macular edema worsening.
- Panretinal photocoagulation. This laser treatment, also known as scatter laser treatment, can shrink abnormal blood vessels. During the procedure, the areas of the retina away from the macula are treated with scattered laser burns. The burns cause the abnormal new blood vessels to shrink and scar.
It's usually done in your doctor's office or eye clinic in two or more sessions. Your vision will be blurry for about a day after the procedure. Some loss of peripheral vision or night vision after the procedure is possible.
- Vitrectomy. This procedure uses a tiny incision in your eye to remove blood from the middle of the eye (vitreous) and scar tissue tugging on the retina. It's done in a surgery center or hospital using local or general anesthesia.
While treatment can slow or stop the progression of diabetic retinopathy, it's not a cure. Because diabetes is a lifelong condition, future retinal damage and vision loss are still possible.
Even after treatment for diabetic retinopathy, you'll need regular eye exams. At some point, you might need additional treatment.
Astigmatism
Astigmatism is a common and generally treatable imperfection in the curvature of the eye that causes blurred distance and near vision.(16)
Astigmatism occurs when either the front surface of the eye (cornea) or the lens inside the eye has mismatched curves.
Symptoms
Signs and symptoms of astigmatism may include:(16)
- Blurred or distorted vision
- Eyestrain or discomfort
- Headaches
- Difficulty with night vision
- Squinting
Treatment
The goal of treating astigmatism is to improve vision clarity and eye comfort. Treatments are corrective lenses or refractive surgery.(17)
Corrective lenses
Wearing corrective lenses treats astigmatism by counteracting uneven curvatures of your cornea or lens.
Types of corrective lenses include:(16,18)
- Eyeglasses are made with lenses that help compensate for the uneven shape of the eye. The lenses make the light bend into the eye properly. Eyeglasses can also correct for other refractive errors, such as nearsightedness or farsightedness.
- Contact lenses. Like eyeglasses, contact lenses can correct most astigmatism. They are available in a variety of types and styles.
Cataract
A cataract develops when the lens in your eye, which is normally clear, becomes foggy.
For your eye to see, light passes through a clear lens. The lens is behind your iris (the colored part of your eye). The lens focuses the light so that your brain and eye can work together to process information into a picture. (19)
When a cataract clouds over the lens, your eye can’t focus light in the same way. This leads to blurry vision or other vision loss (trouble seeing). Your vision change depends on the cataract’s location and size.
Most people start getting cataracts around age 40. But you probably won’t notice symptoms until after age 60. Rarely, babies are born with cataracts due to a birth defect.
You’re more likely to develop cataracts if you:(18)
- Smoke cigarettes.
- Live in an area with bad air pollution.
- Use alcohol heavily.
- Have a family history of cataracts.
Symptoms of Cataracts
Common symptoms of cataracts include:(19)
- blurry vision
- trouble seeing at night
- seeing colors as faded
- increased sensitivity to glare
- halos surrounding lights
- double vision in the affected eye
- a need for frequent changes in prescription glasses
Treatment of Cataracts(20)
If you’re unable or uninterested in surgery, your doctor may be able to help you manage your symptoms. They may suggest stronger eyeglasses, magnifying lenses, or sunglasses with an anti-glare coating.
Surgery(20)
Surgery is recommended when cataracts prevent you from going about your daily activities, such as reading or driving. It’s also performed when cataracts interfere with the treatment of other eye problems.
One surgical method, known as phacoemulsification, involves the use of ultrasound waves to break the lens apart and remove the pieces.
Extracapsular surgery involves removing the cloudy part of the lens through a long incision in the cornea. After surgery, an artificial intraocular lens is placed where the natural lens was.
Surgery to remove a cataract is generally very safe and has a high success rate. Some of the risks of cataract surgery include infection, bleeding, and retinal detachment, though incidences of all those complications are less than 1%. Most people can go home on the same day as their surgery.
Your eyes are complex organs that need many different vitamins and nutrients to function properly.
Though a variety of different factors cause these conditions, nutrition seems to have an influence on all of them — at least in part.(21)
Here are vitamins and nutrients that help maintain eye health.
- Vitamin A
Vitamin A plays a crucial role in vision by maintaining a clear cornea, which is the outside covering of your eye.
This vitamin is also a component of rhodopsin, a protein in your eyes that allows you to see in low-light conditions.
Vitamin A deficiency is rare in developed countries, but if unaddressed, it can lead to a serious condition called xerophthalmia.
Xerophthalmia is a progressive eye disease that begins with night blindness. If vitamin A deficiency continues, your tear ducts and eyes can dry out. Eventually, your cornea softens, resulting in irreversible blindness.
For general eye health, vitamin-A-rich foods are recommended over supplements. Sweet potatoes are an excellent source, as are leafy green vegetables, pumpkins, and bell peppers. (21)
- Vitamin E
Vitamin E is a potent antioxidant that helps protect your cells — including your eye cells — from damage by harmful free radicals and unstable molecules.
Some studies suggest that diets high in vitamin E may help prevent age-related cataracts.(21)
A diet with adequate vitamin E is recommended to maintain eye health. Some vitamin E-rich options include nuts, seeds, and cooking oils. Salmon, avocado, and leafy green vegetables are also useful sources.
- Vitamin C
Vitamin C is a powerful antioxidant that may protect your eyes against damaging free radicals.
Vitamin C is required to make collagen, a protein that provides structure to your eye, particularly in the cornea and sclera.
Citrus and tropical fruits, bell peppers, broccoli, and kale contain particularly excessive amounts of vitamin C, making them great options to boost your daily intake.(21)
Makkah Pharmacy recommends:
-
- Vitamins B6, B9, and B12
This combination of vitamins can lower levels of homocysteine, a protein in your body that may be associated with inflammation and an increased risk of developing AMD.
A clinical study in women demonstrated a 34% reduced risk of developing AMD while taking 1,000 mcg of vitamin B12 along with vitamins B6 and B9.(21)
- Omega-3 Fatty Acids
Omega-3 fatty acids are a type of polyunsaturated fat. The cell membranes of your retina contain a high concentration of docosahexaenoic acid (DHA), a particular type of omega-3.
Besides helping form the cells of your eye, omega-3 fats have anti-inflammatory properties, which may play a role in the prevention of diabetic retinopathy.
Omega-3 fats may also benefit individuals with dry eye disease by helping them produce more tears. With this condition, a lack of tears causes dryness, discomfort, and occasional blurry vision.(21)
To increase omega-3 fatty acids in your diet, include rich sources such as fish, flaxseed, chia seeds, soy, and nuts. Omega-3s can also be found in cooking oils such as canola and olive oil.
References:
- The Eyes (Human Anatomy): Diagram, Optic Nerve, Iris, Cornea, Pupil, & More [Internet]. [cited 2022 Nov 19]. Available from: https://www.webmd.com/eye-health/picture-of-the-eyes
- Eyes: How They Work, Anatomy & Common Conditions [Internet]. [cited 2022 Nov 19]. Available from: https://my.clevelandclinic.org/health/body/21823-eyes
- Age-Related Macular Degeneration [Internet]. [cited 2022 Nov 19]. Available from: https://www.webmd.com/eye-health/macular-degeneration/age-related-macular-degeneration-overview
- Signs and Symptoms of Macular Degeneration [Internet]. [cited 2022 Nov 19]. Available from: https://www.webmd.com/eye-health/macular-degeneration/age-related-macular-degeneration-symptoms
- Age-Related Macular Degeneration Treatment [Internet]. [cited 2022 Nov 19]. Available from: https://www.webmd.com/eye-health/macular-degeneration/age-related-macular-degeneration-treatment
- Dry eyes - Symptoms and causes - Mayo Clinic [Internet]. [cited 2022 Nov 19]. Available from: https://www.mayoclinic.org/diseases-conditions/dry-eyes/symptoms-causes/syc-20371863
- Martin E, Oliver KM, Pearce EI, Tomlinson A, Simmons P, Hagan S. Effect of tear supplements on signs, symptoms and inflammatory markers in dry eye. Cytokine. 2018 May 1;105:37–44.
- Dry eyes - Diagnosis and treatment - Mayo Clinic [Internet]. [cited 2022 Nov 19]. Available from: https://www.mayoclinic.org/diseases-conditions/dry-eyes/diagnosis-treatment/drc-20371869
- Martin E, Oliver KM, Pearce EI, Tomlinson A, Simmons P, Hagan S. Effect of tear supplements on signs, symptoms and inflammatory markers in dry eye. Cytokine. 2018 May 1;105:37–44.
- Glaucoma: Causes, Types, Symptoms, Diagnosis, and Treatment [Internet]. [cited 2022 Nov 19]. Available from: https://www.webmd.com/eye-health/glaucoma-eyes
- Glaucoma - Symptoms, and causes - Mayo Clinic [Internet]. [cited 2022 Nov 19]. Available from: https://www.mayoclinic.org/diseases-conditions/glaucoma/symptoms-causes/syc-20372839
- Glaucoma - Diagnosis and treatment - Mayo Clinic [Internet]. [cited 2022 Nov 19]. Available from: https://www.mayoclinic.org/diseases-conditions/glaucoma/diagnosis-treatment/drc-20372846
- Diabetic Retinopathy: How to Prevent Vision Loss [Internet]. [cited 2022 Nov 19]. Available from: https://www.webmd.com/diabetes/diabetic-retinopathy
- Diabetic retinopathy - Symptoms and causes - Mayo Clinic [Internet]. [cited 2022 Nov 19]. Available from: https://www.mayoclinic.org/diseases-conditions/diabetic-retinopathy/symptoms-causes/syc-20371611
- Diabetic retinopathy - Diagnosis and treatment - Mayo Clinic [Internet]. [cited 2022 Nov 19]. Available from: https://www.mayoclinic.org/diseases-conditions/diabetic-retinopathy/diagnosis-treatment/drc-20371617
- Astigmatism - Symptoms and causes - Mayo Clinic [Internet]. [cited 2022 Nov 19]. Available from: https://www.mayoclinic.org/diseases-conditions/astigmatism/symptoms-causes/syc-20353835
- Keshav V, Henderson BA. Astigmatism Management with Intraocular Lens Surgery. Ophthalmology. 2021 Nov 1;128(11):e153–63.
- Cataracts: What They Are, Causes, Symptoms, Surgery, Recovery Time [Internet]. [cited 2022 Nov 19]. Available from: https://my.clevelandclinic.org/health/diseases/8589-cataracts
- Cataract: Types, Causes and Risk Factors [Internet]. [cited 2022 Nov 19]. Available from: https://www.healthline.com/health/cataract#symptoms
- Cataract: Types, Causes and Risk Factors [Internet]. [cited 2022 Nov 19]. Available from: https://www.healthline.com/health/cataract#treatments
- The Top 9 Best Vitamins for Eye Health [Internet]. [cited 2022 Nov 19]. Available from: https://www.healthline.com/nutrition/eye-vitamins